The following experiences from the final stages of life of my loved ones have raised some important questions:
When my mother was once discharged from the Intensive Care Unit (ICU), she told us, “My dear children, please don’t put me in the ICU again—I feel so lonely and abandoned.” Yet, despite her plea, we had no choice but to admit her to the ICU several more times before she passed away in 2005. Does an individual have the right to specify what should not be done in their medical care?
A close relative of mine in his eighties, diagnosed with a terminal illness, took a sudden turn for the worse. A doctor, an expert in the condition, and a close family acquaintance predicted he had only three days left to live. However, his suffering continued for three long years. During that time, he was fed through a tube, had a urinary catheter, and his hands were tied to the bed rails, so he wouldn’t pull out the tubes unknowingly- until he passed away in 2022. Would he, as a doctor himself, in hindsight, have chosen to extend his life in this manner on supports knowing the quality of life left?
This raises an important question: Can individuals express their preferences or make choices in advance regarding their future medical care?
The answer is YES. The Living will
Today, there is a growing trend in the healthcare industry to offer increasingly expensive treatments, with hospitals competing against each other. In cancer treatment, for example, more hospitals are establishing oncology departments and providing treatments that are not only costly but also physically demanding, often compromising the patient’s quality of life, with an indefinite chance for survival.
In advanced countries, such treatments are administered only after a thorough evaluation by a medical team, ensuring a high probability of success. Even after treatment begins, it is discontinued if no positive impact is observed. A reality check is conducted and shared with the patient and their family, and in such cases, care shifts to palliative centers or hospices.
In India, however, families are often pressured to continue spending on treatment—driven by the recommendations of doctors, hospital demands, and societal expectations. In the end, they lose their loved one after exhausting significant financial resources.
Can an individual determine in advance the extent and limits of medical treatment they receive in such situations?
The answer is YES. The Living will
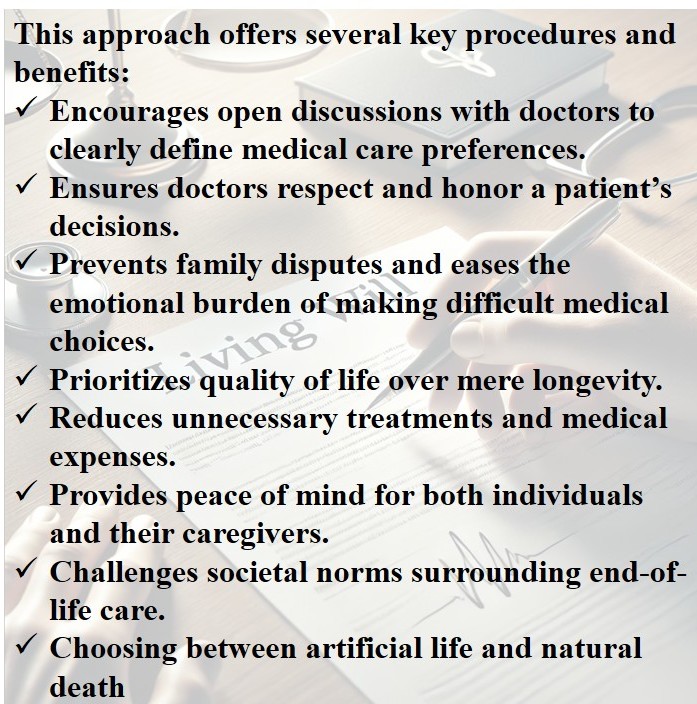
An Advance Medical Directive / Living Will documented by an individual can help define the extent of treatment an individual wishes to receive, preventing unnecessary financial and emotional burdens on family members.
A living Will has been legally recognized in India since 2018, following a Supreme Court ruling that established a process for terminally ill patients with no hope of recovery to withhold or withdraw medical treatment and pass away with dignity. Since patients may be unable to express their wishes due to conditions such as unconsciousness or dementia, living will allow them to make decisions about their future medical care in advance.
Also known as an Advance Medical Directive, a living will is a vital tool that upholds the fundamental right to live—and die—with dignity. It serves as a written declaration of a person’s medical preferences, ensuring that designated individuals or family members can honor their wishes without guilt or conflict during a critical time.
In 2023, the Supreme Court simplified creating a living will. Now, individuals can complete a standardized form expressing their desire to discontinue medical treatment if necessary. This document must be witnessed and attested by a gazette officer.
Anyone over the age of 18, while in good health and sound mind, can create a living will. If a person is later diagnosed with a terminal illness or enters a persistent vegetative state with no possibility of recovery, the will can be enacted to discontinue further medical intervention.

Safeguards: To ensure the legitimacy of a living will and prevent misuse, government guidelines mandate approval from two medical committees before its implementation. One committee, consisting of three doctors, is formed within the hospital where the patient is admitted, while the other is constituted by the district medical officer.
Dying with Dignity: Breaking the Taboo Around ‘Living Wills’ in India
—this was the headline of a BBC report on February 3, 2025. Despite being called a “Living Will,” the document deals with end-of-life decisions, a topic considered taboo in Indian culture. Overcoming this cultural barrier is crucial to encouraging people to take action on living wills.
According to the BBC report, Kerala took the lead in this groundbreaking initiative. In November 2024, Dr. Yadev and his team launched India’s first program at the Government Medical College in Kollam district to educate the public about living wills. The initiative provides information both in person and over the phone, while volunteers conduct awareness campaigns and distribute will templates.



Kochouseph has highlighted the main constraint we Indians face: “the pressure of societal expectations on patient treatment.” By openly sharing his living will with family and friends, he has broken free from this restraint. His decision serves as a powerful advocacy tool, promoting awareness and encouraging others to consider the importance of a living will.
The concept of a Living Will reinforces a fundamental truth: as individuals, we have the right to live and die with dignity. With this right comes the responsibility of making informed decisions about our medical treatment. Autonomy, self-determination, and clarity are essential in shaping these choices.


Leave a comment